New Study Evaluates the Ability of Masimo SedLine® Brain Function Monitoring to Predict Neurological Outcomes and Long-term Survival in Post-Cardiac Arrest ICU Patients
Masimo (NASDAQ: MASI) has released findings from a study in the Journal of Critical Care showing that two parameters from Masimo SedLine®—Patient State Index (PSi) and Suppression Ratio (SR)—can accurately predict neurological outcomes and long-term survival in post-cardiac arrest ICU patients. The study indicates that low values of PSi and SR correlate with higher mortality rates at 180 days, establishing their effectiveness as prognostic tools. This may influence treatment plans and care decisions in critical care settings.
- PSi and SR show high predictability for mortality 180 days after cardiac arrest.
- Combination of PSi and SR offers better prognostic accuracy than individual parameters.
- None.
Insights
Analyzing...
Masimo (NASDAQ: MASI) announced today the findings of a study published in the Journal of Critical Care in which Dr. Tae Youn Kim and colleagues at the Dongguk University College of Medicine and Yonsei University College of Medicine in Korea evaluated the ability of two parameters provided by Masimo SedLine® brain function monitoring to predict neurological outcomes and long-term survival in post-cardiac arrest ICU patients.1 The researchers found that the combination of the two parameters, Patient State Index (PSi) and Suppression Ratio (SR) had “high predictability” for mortality 180 days after cardiac arrest.
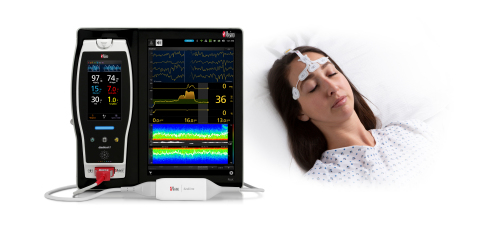
Masimo SedLine® Brain Function Monitoring (Photo: Business Wire)
Noting that “accurate prognostication” in post-cardiac arrest patients is important to determine treatment plans and “whether to continue or withdraw intensive care,” and that a “multi-modal” approach is recommended because “no single prognostic factor has been shown to have higher prognostic accuracy than those of other factors,” the researchers sought to evaluate the prognostic accuracy of the two Masimo SedLine parameters as predictors of neurological outcomes, both alone and in combination. The researchers chose PSi because, as they note, raw EEG data can be “difficult to use” and PSi, which is derived from EEG, is widely used in anesthesiology for determining the degree of procedural sedation, “significantly co-varies with changes in the state” under general anesthesia, and “can significantly predict” the level of arousal in varying stages of anesthetic delivery. The researchers chose SR because it helps to estimate the percentage of EEG suppression and is therefore considered a good predictor of poor neurologic outcomes.2
They enrolled 103 adult patients between January 2017 and August 2020 who experienced a non-traumatic out-of-hospital cardiac arrest, had been successfully resuscitated after CPR, and received targeted temperature management during their ICU stay. PSi and SR were continuously monitored using Masimo SedLine from immediately after ICU admission until 24 hours after return of spontaneous circulation (ROSC), recorded at one hour intervals. Neurological outcomes were categorized using the Pittsburgh Brain Stem Score (PBSS) and Cerebral Performance Category (CPC). Data on survival at 180 days was obtained via telephonic interviews.
The researchers found that using either PSi or SR alone had “good predictability” for poor neurological outcome, and that the combination of low PSi and SR had “high predictability” for mortality 180 days after cardiac arrest. They used receiver operating characteristic (ROC) curves to determine that “a mean PSI ≤ 14.53 and mean SR > 36.6 showed high diagnostic accuracy” as single prognostic factors for patients in their study. Furthermore, “Multimodal prediction using the mean PSi and mean SR showed the highest area-under-the-curve value of 0.965 (
The researchers concluded that “PSi and SR are good predictors for early neuro-prognostication in post-cardiac arrest patients.” They also noted, “The combination of PSI and SR showed better predictability of poor neurologic outcome than did each individual parameter.”
@Masimo | #Masimo
About Masimo
Masimo (NASDAQ: MASI) is a global medical technology company that develops and produces a wide array of industry-leading monitoring technologies, including innovative measurements, sensors, patient monitors, and automation and connectivity solutions. Our mission is to improve patient outcomes, reduce the cost of care, and take noninvasive monitoring to new sites and applications. Masimo SET® Measure-through Motion and Low Perfusion™ pulse oximetry, introduced in 1995, has been shown in over 100 independent and objective studies to outperform other pulse oximetry technologies.3 Masimo SET® has also been shown to help clinicians reduce severe retinopathy of prematurity in neonates,4 improve CCHD screening in newborns,5 and, when used for continuous monitoring with Masimo Patient SafetyNet™ in post-surgical wards, reduce rapid response team activations, ICU transfers, and costs.6-9 Masimo SET® is estimated to be used on more than 200 million patients in leading hospitals and other healthcare settings around the world,10 and is the primary pulse oximetry at 9 of the top 10 hospitals according to the 2020-21 U.S. News and World Report Best Hospitals Honor Roll.11 Masimo continues to refine SET® and in 2018, announced that SpO2 accuracy on RD SET® sensors during conditions of motion has been significantly improved, providing clinicians with even greater confidence that the SpO2 values they rely on accurately reflect a patient’s physiological status. In 2005, Masimo introduced rainbow® Pulse CO-Oximetry technology, allowing noninvasive and continuous monitoring of blood constituents that previously could only be measured invasively, including total hemoglobin (SpHb®), oxygen content (SpOC™), carboxyhemoglobin (SpCO®), methemoglobin (SpMet®), Pleth Variability Index (PVi®), RPVi™ (rainbow® PVi), and Oxygen Reserve Index (ORi™). In 2013, Masimo introduced the Root® Patient Monitoring and Connectivity Platform, built from the ground up to be as flexible and expandable as possible to facilitate the addition of other Masimo and third-party monitoring technologies; key Masimo additions include Next Generation SedLine® Brain Function Monitoring, O3® Regional Oximetry, and ISA™ Capnography with NomoLine® sampling lines. Masimo’s family of continuous and spot-check monitoring Pulse CO-Oximeters® includes devices designed for use in a variety of clinical and non-clinical scenarios, including tetherless, wearable technology, such as Radius-7® and Radius PPG™, portable devices like Rad-67®, fingertip pulse oximeters like MightySat® Rx, and devices available for use both in the hospital and at home, such as Rad-97®. Masimo hospital automation and connectivity solutions are centered around the Masimo Hospital Automation™ platform, and include Iris® Gateway, iSirona™, Patient SafetyNet, Replica™, Halo ION™, UniView®, UniView :60™, and Masimo SafetyNet™. Additional information about Masimo and its products may be found at www.masimo.com. Published clinical studies on Masimo products can be found at www.masimo.com/evidence/featured-studies/feature/.
ORi and RPVi have not received FDA 510(k) clearance and are not available for sale in the United States. The use of the trademark Patient SafetyNet is under license from University HealthSystem Consortium.
References
- Kim TY, Hwang SO, Jung WJ, et al. Early neuroprognostication with the Patient State Index and suppression ratio in post-cardiac arrest patients. J Crit Care. 2018. https://doi.org/10.1016/j.jcrc.2020.06.003.
- Seder DB, Fraser GL, Robbins T, Libby L, Riker RR. The bispectral index and suppression ratio are very early predictors of neurological outcome during therapeutic hypothermia after cardiac arrest. Intensive Care Med 2010;36(2):281-8.
- Published clinical studies on pulse oximetry and the benefits of Masimo SET® can be found on our website at http://www.masimo.com. Comparative studies include independent and objective studies which are comprised of abstracts presented at scientific meetings and peer-reviewed journal articles.
- Castillo A et al. Prevention of Retinopathy of Prematurity in Preterm Infants through Changes in Clinical Practice and SpO2 Technology. Acta Paediatr. 2011 Feb;100(2):188-92.
- de-Wahl Granelli A et al. Impact of pulse oximetry screening on the detection of duct dependent congenital heart disease: a Swedish prospective screening study in 39,821 newborns. BMJ. 2009;Jan 8;338.
- Taenzer A et al. Impact of pulse oximetry surveillance on rescue events and intensive care unit transfers: a before-and-after concurrence study. Anesthesiology. 2010:112(2):282-287.
- Taenzer A et al. Postoperative Monitoring – The Dartmouth Experience. Anesthesia Patient Safety Foundation Newsletter. Spring-Summer 2012.
- McGrath S et al. Surveillance Monitoring Management for General Care Units: Strategy, Design, and Implementation. The Joint Commission Journal on Quality and Patient Safety. 2016 Jul;42(7):293-302.
- McGrath S et al. Inpatient Respiratory Arrest Associated With Sedative and Analgesic Medications: Impact of Continuous Monitoring on Patient Mortality and Severe Morbidity. J Patient Saf. 2020 14 Mar. DOI: 10.1097/PTS.0000000000000696.
- Estimate: Masimo data on file.
- http://health.usnews.com/health-care/best-hospitals/articles/best-hospitals-honor-roll-and-overview.
Forward-Looking Statements
This press release includes forward-looking statements as defined in Section 27A of the Securities Act of 1933 and Section 21E of the Securities Exchange Act of 1934, in connection with the Private Securities Litigation Reform Act of 1995. These forward-looking statements include, among others, statements regarding the potential effectiveness of Masimo SedLine®. These forward-looking statements are based on current expectations about future events affecting us and are subject to risks and uncertainties, all of which are difficult to predict and many of which are beyond our control and could cause our actual results to differ materially and adversely from those expressed in our forward-looking statements as a result of various risk factors, including, but not limited to: risks related to our assumptions regarding the repeatability of clinical results; risks related to our belief that Masimo's unique noninvasive measurement technologies, including Masimo SedLine, contribute to positive clinical outcomes and patient safety; risks related to our belief that Masimo noninvasive medical breakthroughs provide cost-effective solutions and unique advantages; risks related to COVID-19; as well as other factors discussed in the "Risk Factors" section of our most recent reports filed with the Securities and Exchange Commission ("SEC"), which may be obtained for free at the SEC's website at www.sec.gov. Although we believe that the expectations reflected in our forward-looking statements are reasonable, we do not know whether our expectations will prove correct. All forward-looking statements included in this press release are expressly qualified in their entirety by the foregoing cautionary statements. You are cautioned not to place undue reliance on these forward-looking statements, which speak only as of today's date. We do not undertake any obligation to update, amend or clarify these statements or the "Risk Factors" contained in our most recent reports filed with the SEC, whether as a result of new information, future events or otherwise, except as may be required under the applicable securities laws.
View source version on businesswire.com: https://www.businesswire.com/news/home/20210705005314/en/







